Your retina is located at the back of your eye. Although it is a thin, light-sensitive tissue, it packs a punch: it is responsible for controlling how you see images. In an ideal eye, images focus on the retina and those images are converted into electrical impulses that are transmitted through the optic nerve to the brain. It makes sense, then, that any damage to the retina will result in vision problems ranging from blurriness to spots to decreased central vision and even blindness.
Types of Retinal Diseases
There are many different types of retinal diseases including, but not limited to:
- Macular degeneration
- Retinal tears or detachment
- Diabetic retinopathy
- Retinal vein occlusion
- Macular edema
- Macular holes or puckers
- Flashes and floaters
At Atwal Eye Care, our doctors offer diagnosis and treatment for retinal diseases. The treatment will depend on which part of the retina is affected, how severe the problem is and what is causing the problem. A comprehensive dilated eye exam will help your doctor diagnose the issue and recommend treatment options.
Learn more about some of the retina conditions we treat:
- Central Serous Retinopathy
- Choroidal Nevus
- Flashes & Floaters
- Macular Edema
- Macular Holes and Puckers
- Posterior Vitreous Detachment
- Retinal Artery Occlusion
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Uveitis
- Vitrectomy
Central Serous Retinopathy
When fluid builds up behind the retina, it can cause the retina to detach from the back of the eye. When this occurs in the central part of the retina, this is called central serous retinopathy.
Symptoms of Central Serous Retinopathy
Central serous retinopathy does not always have obvious symptoms. However, some patients may experience:
- Sudden or gradual vision loss
- Blurry vision in one eye
- Dark spot in central vision
- Straight lines appear wavy
- Dullness in color vision
Risk Factors for Central Serous Retinopathy
Central serous retinopathy typically affects men between the ages of 30 and 50, but women can also develop the condition. Other risk factors include:
- Aging
- Stress
- Medications that cause inflammation such as corticosteroids
- Caucasian race
While you cannot stop the aging process, lifestyle changes to reduce stress can reduce these risks: getting plenty of sleep, exercising, limiting alcohol and caffeine, etc.
Treatment for Central Serous Retinopathy
Treatment for this condition is not always necessary. The fluid may simply drain on its own. However, this is not a condition that you should self-diagnose or ignore. Regular eye exams will allow your doctor to monitor the condition. If your fluid is being stubborn, your doctor may recommend:
- Medications (or the halting of medications): anti-vascular endothelial growth factor medications may help prevent fragile blood vessels from forming on the retina; steroid medication use should be stopped
- Photodynamic therapy: the combination of the drug verteporfin and a cool laser is used to stop the leak and prevent future leaks
- Thermal laser treatment: performed to seal the leak
Choroidal Nevus
A choroidal nevus is basically a freckle inside your eye. People are not typically born with a choroidal nevus; they can develop over time. They are caused by the clumping of cells called melanocytes, the melanin pigment that colors our skin, hair and eyes. This is not something that you can see just by looking at your eyes; however, your eye doctor will be able to diagnose and monitor the condition of the eye nevus. In most cases, these are benign and do not need to be treated. However, if it begins leaking fluid, changes to an orange color (they are typically grey/brown/yellow) or begins to thicken, those may be signs that it is a malignant choroidal melanoma.
Symptoms of Choroidal Nevus
If the choroidal nevus is normal, you may not know it is even present until an eye doctor discovers it. However, if it begins to change as noted above, you may begin to experience symptoms such as flashes of light or vision loss. Signs that you have a retinal detachment due to an eye freckle may include:
- Floaters
- Flashes
- Reduced peripheral vision
- Shadow over your visual field
- Blurry vision
Treatment for Choroidal Nevus
There is no way to safely remove a choroidal nevus. If your condition turns into choroidal melanoma, your doctor will closely monitor your condition and may recommend radiation therapy. In extreme cases, enucleation (removal of the eye) may be recommended.
Flashes and Floaters
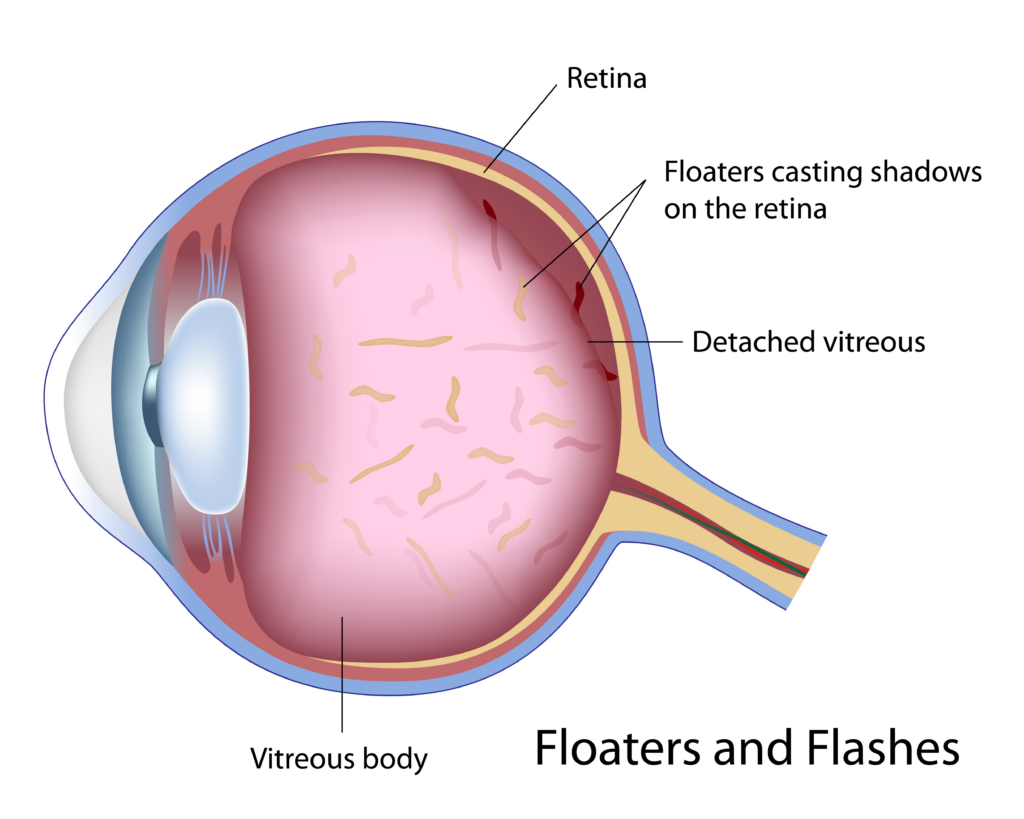
Flashes and floaters are related to the clear vitreous gel inside your eye. Over time, the vitreous can clump, thicken or shrink within the eye, leading to interruptions in your vision. These conditions are occurring inside your eye.
- Flashes: vitreous gel rubs against your retina or causes a tear in your retina
- Floaters: vitreous gel clumps or forms strands that cause shadows to move across your field of vision
Floaters are different from eye gunk that you may clean out of your eyes each morning or throughout the day.
Symptoms of Flashes & Floaters
The symptoms of flashes and floaters can come and go.
- Dots, lines or cobwebs in your vision
- Sudden flashes of light, like seeing stars
- Disturbance in peripheral vision
- Dark shadow over your vision
Risk Factors for Flashes & Floaters
- Nearsightedness
- Previous cataract surgery
- Inflammation within the eye
- Eye trauma
- Aging
- Migraine headaches
Treatment for Flashes & Floaters in Buffalo, NY
These are not typically serious vision problems that require treatment. However, if you experience an abundance of these symptoms, especially all at once, schedule an eye exam right away. It is important to have a doctor monitor your condition to ensure there is no vitreous detachment, retina tear or full retinal detachment. This would signify a medical emergency. A retinal detachment may be treated in any number of ways:
- Vitrectomy: the vitreous gel in the eye is drained and replaced with a gas bubble to reduce retinal pulling due to the changes in vitreous gel
- Pneumatic retinopexy: a gas bubble is injected into the vitreous gel to push the tear into proper position on the retinal wall
- Scleral buckle: a flexible silicone band is placed around the eye to relieve pressure caused by the shrinking and contracting of the vitreous gel
- Retina laser surgery: the retina is connected back in proper position using tiny burns
- Cryopexy: intense cold is applied to the retinal tear that produces a scar to reattach the retina
If you are experiencing eye floaters, contact us to schedule a comprehensive eye exam to prevent permanent vision loss.
Macular Edema
When fluid builds up behind the macula (the central part of the retina), causing the area to thicken and enlarge, this is called macular edema. Damaged blood vessels are often the reasons why fluid can accumulate in this area. The condition is often associated with diabetics because of the ongoing damage that occurs to the blood vessels in the eyes, resulting in diabetic macular edema.
Symptoms of Macular Edema
- Wavy central vision
- Blurry vision
- Faded color perception
- Vision loss
Risk Factors for Macular Edema
- Diabetes/diabetic retinopathy
- Wet age-related macular degeneration
- Inflammatory diseases (uveitis)
- Previous eye surgery
- Retinal vein occlusion
Treatment for Macular Edema
The right treatment will depend on the root cause and severity of your condition:
- Medications: steroids or anti-VEGF (vascular endothelial growth factor) injections to reduce the risk of abnormal blood vessel growth
- Anti-inflammatory treatments: corticosteroid treatments in the form of eye drops, oral medication or injections may help reduce inflammation
- Laser treatment: laser burns are performed to stop leaks of fluid and blood or to shrink abnormal blood vessels
- Vitrectomy: blood vessels, blood and scar tissue are removed from the vitreous gel in the eye
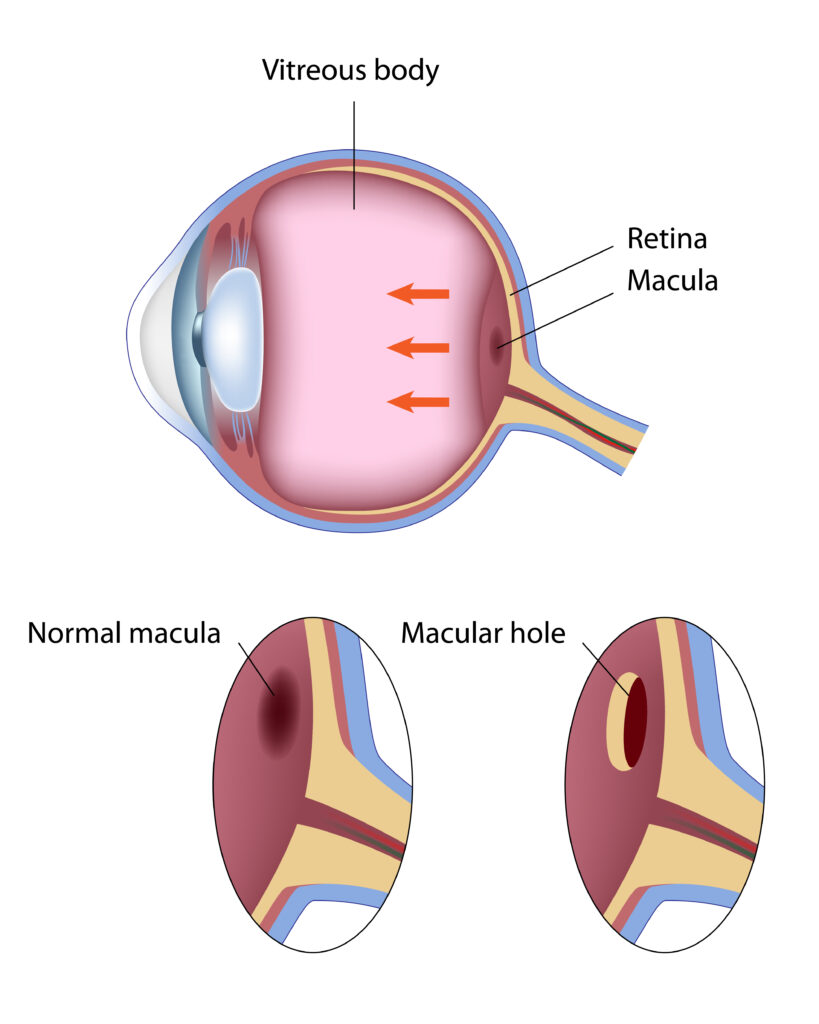
Macular Holes and Puckers
Your macula is the part of your eye that allows you to have central vision. Located in the center of the retina, this collection of nerve cells is the location where the eye focuses on images. If there is any break in the nerve cell fibers, you can develop what is called a macular hole. If scar tissue begins to grow over this same area, it is called a macular pucker.
Symptoms of Macular Holes and Puckers
- Loss of central vision
- Distortion of central vision
- Straight lines appear wavy
- Gray spot or blind spot in central vision
Macular holes can cause more serious vision problems or vision loss over time than macular puckers. The severity of the hole (partial thickness or full thickness) will have a big impact on your vision. Neither condition is typically associated with pain, but if you notice any of these symptoms, it is important to see an eye doctor to get the condition under control.
Causes of Macular Holes and Puckers
Macular holes are more common in women, especially those over age 60, but they can occur in men as well. A macular pucker can cause a hole to develop. This condition can also be caused by:
- Diabetic eye disease
- Detached retina
- Eye trauma or injury
- Extreme myopia (nearsightedness)
Your eye is filled with a jelly-like substance called the vitreous. If this substance shrinks, it can detach from the retina surface, leading to the formation of scar tissue. When this occurs on the macula, you develop a macular pucker and your central vision will be disrupted.
Treatment for Macular Holes and Puckers
The common treatment for a macular hole is vitrectomy surgery. During this procedure, doctors remove the vitreous gel from your eye and replace it with an air or gas bubble. The bubble allows the edges of the holes to come together, allowing it to heal. The bubble evaporates naturally and the eye refills itself with its own saline fluid.
Macular puckers often do not require any treatment unless the condition is seriously affecting your vision. If treatment is necessary, the vitreous gel is removed and replaced with a saline solution. Scar tissue can also be removed.
Posterior Vitreous Detachment
Vitreous is a gel-like substance that fills the inside of your eye and attaches to the retina (the back of the eye). It is normal for this vitreous to shrink as you age, causing the millions of tiny fibers inside the vitreous to pull on the retina. If the vitreous pulls away from the retina, this is called a posterior vitreous detachment. This is a common condition in people over age 50, especially if you are nearsighted.
Symptoms of Posterior Vitreous Detachment
There are often no symptoms of a posterior vitreous detachment and it may not affect your vision. However, some people do experience symptoms such as:
- Flashes of light in your peripheral vision
- Floaters that look like cobwebs or dark spots in your vision
- Shadows that dart around your vision
Side Effects of Posterior Vitreous Detachment
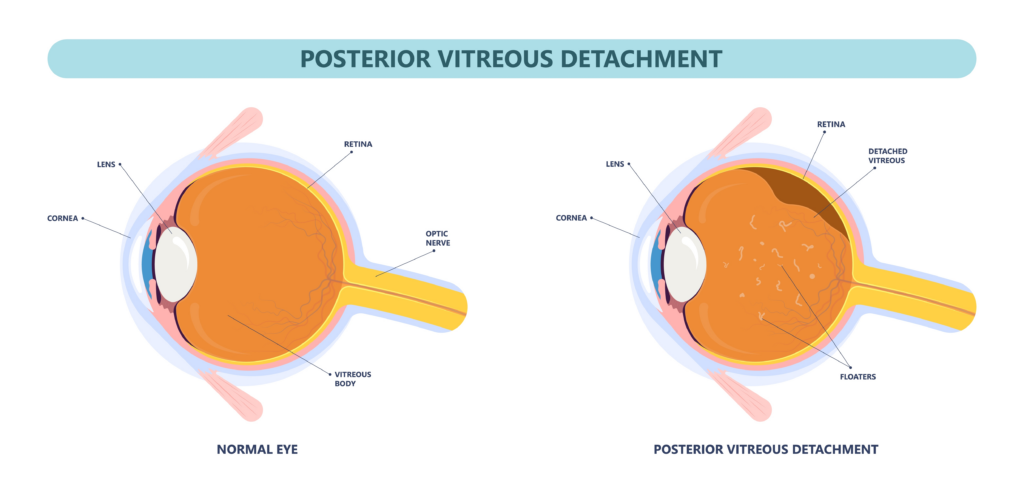
A posterior vitreous detachment may not threaten your vision. However, it is possible for this condition to lead to a tear in your retina, retinal detachment or a pucker or hole in your macula (the center of your retina). Any of these conditions will threaten your sight and must be treated immediately. If you experience any of the above symptoms, we recommend you schedule an eye exam right away, just to be on the safe side.
Treatment for Posterior Vitreous Detachment
Your doctor will want to perform regular dilated eye exams to monitor the posterior vitreous detachment and ensure that there is no serious retinal damage. While treatment may not be necessary for a posterior vitreous detachment, your doctor will definitely treat any new condition that develops such as a retinal detachment, macular hole, etc. Our doctors may recommend laser surgery, cryotherapy (freezing), vitrectomy or another treatment.
Retinal Artery Occlusion
The network of arteries in your retina carry oxygen to your nerve cells. Any time there is a blockage in these arteries (from cholesterol or a blood clot, for example), you could experience vision loss. This is called retinal artery occlusion. Not surprisingly, if the main artery becomes blocked, you will suffer more severe vision loss (central retinal artery occlusion). It is also possible for a smaller artery to become blocked (branch retinal artery occlusion) without your knowledge because there can be little to no visual disturbance.
Symptoms of Retinal Artery Occlusion
It is possible for the blockage to be temporary and go unnoticed, especially because the condition is usually painless. However, the sudden loss of vision in one eye could signify a more permanent blockage.
Risk Factors for Retinal Artery Occlusion
- Aging
- Fatty deposits in the arteries
- Diabetes
- Pregnancy or oral contraceptives
- Intravenous drug use
- Carotid artery disease
- Heart disease, tumors in the heart or abnormal heartbeat
- High blood pressure
- Blood clots from the neck artery or heart
Treatment for Retinal Artery Occlusion
While there is no medical treatment for retinal artery occlusion, there are techniques that can be done to dislodge the blockage. These may be effective if they are done very quickly: 4-6 hours after the symptoms start:
- Inhalation of a mixture of 95% oxygen and 5% carbon dioxide to dilate the retinal arteries
- Lower the intraocular pressure with medication or the removal of fluid from the front of the eye (paracentesis)
- Massage of the eye
Retinal Vein Occlusion
Retinal vein occlusion occurs when any of the tiny veins in the retina (the back of the eye) become blocked, often due to the hardening of your arteries and a blood clot. The blockage can occur in in the branch veins or in the main central vein. If blood cannot flow freely from the retina and becomes clogged, this can lead to a build-up of pressure in the blood vessels. If fluid and blood start to leak from the blood vessels, this can damage the retina and affect your vision.
Symptoms of Retinal Vein Occlusion
Some people will not have any symptoms of a retinal vein occlusion; others will experience:
- Blurry vision
- Dark spots/lines in vision
- Sudden permanent blindness
- Eye pain
- Peripheral vision loss
By having regular eye exams, your doctor can diagnose this condition early so your eyesight can be protected. Your doctor will examine the back of your eye to assess the health of your retina.
Risk Factors for Retinal Vein Occlusion
- High blood pressure
- High cholesterol
- Diabetes
- Smoking
- Being overweight
- Glaucoma
- Eye trauma
Treatment for Retinal Vein Occlusion
While there is no medical treatment for retinal vein occlusion, there are techniques that can be done to stabilize your vision:
- Injection of an anti-vascular endothelial growth factor (anti-VEGF) or a steroid to reduce swelling
- Focal laser therapy to close blood vessels near the center of your retina (the macula) using tiny burns
- Laser surgery to stop new blood vessels from growing and leaking blood/fluid
Retinitis Pigmentosa
Your retina contains photoreceptors (rods and cones) that convert light coming into your eyes into electrical signals that travel from the optic nerve to the brain so you can process the images. If there is a breakdown in these cells, your vision will be interrupted.
Retinitis pigmentosa (RP) is a group of genetic disorders that occurs when there are changes in the genes that help your photoreceptor cells make the necessary proteins to function properly. This causes the photoreceptor cells to deteriorate or mutate. Rods are typically affected first, leading to night blindness and loss of vision. As the cones become affected, it will become more challenging to perform normal daily tasks, see color or recognize people or objects.
Symptoms of Retinitis Pigmentosa
Because this is a genetic disorder, people are born with RP. Children may find it hard to maneuver in dark environments, they may be clumsy, they may be sensitive to lights and may have trouble adjusting to changes in lighting. The severity of vision problems will vary from person to person, but RP patients can expect to experience gradual worsening of these symptoms:
- Loss of peripheral (side) vision
- Poor night vision
- Limited vision in dim/dark environments
- Tunnel vision
- Blindness
Risk Factors for Retinitis Pigmentosa
While rare, this disorder can be inherited from parents who pass mutant genes to their children. Not all children will end up having the disorder or being a carrier of the gene (able to pass it down to their own future children). There are several different ways to inherit RP:
- Autosomal recessive inheritance: 2 copies of the mutant gene are necessary to have the disorder or become a carrier
- Autosomal dominant inheritance: 1 copy of the mutant gene is necessary to have the disorder
- X-linked inheritance: passed down by the mother with the mutated gene in one X chromosome, often causing the son to develop the disorder while daughters may become a carrier
Treatment for Retinitis Pigmentosa
RP is estimated to affect 1 in 4,000 people worldwide. Unfortunately, there is no cure for this disorder. People with RP can learn to live with the condition with low vision aids such as magnifying lenses, portable lighting devices, mobility training, guide dogs, etc. Vitamin treatments may also be helpful in slowing the progression of the disorder.
Uveitis
Uveitis is a type of eye inflammation that occurs in the uvea of your eye (the middle layer of tissue). This condition is often caused by an infection, trauma/injury to the eye or an inflammatory disease and it can affect one or both eyes. If left untreated, this condition can lead to vision conditions such as glaucoma, cataracts, retinal detachment and even permanent vision loss.
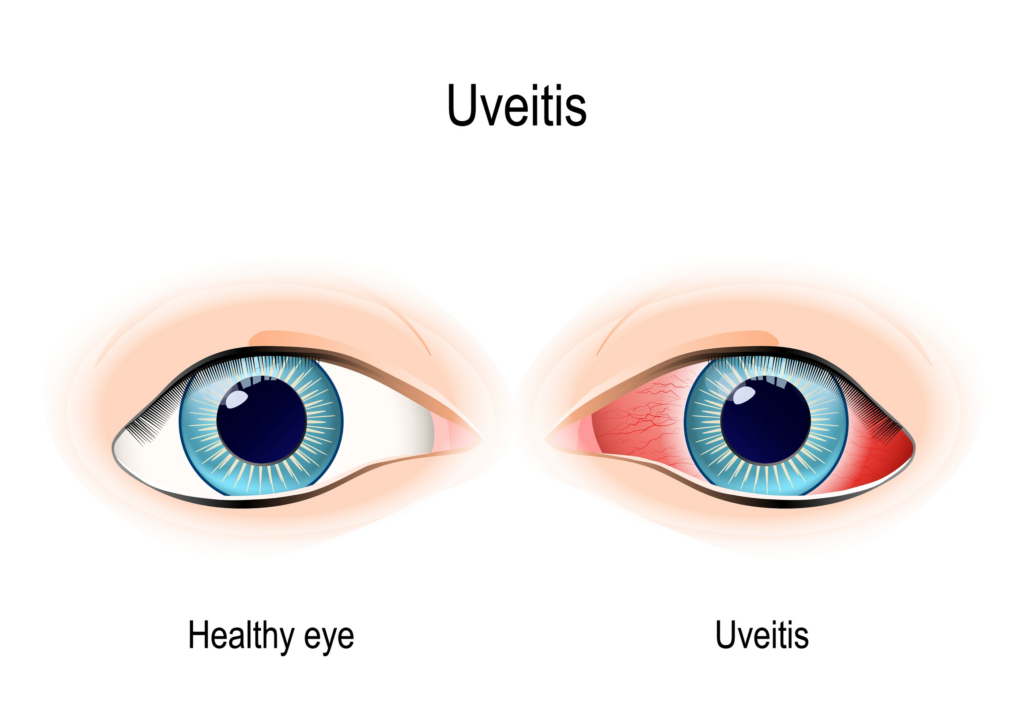
Symptoms of Uveitis
Symptoms may come on suddenly and become more severe very quickly. These symptoms can last weeks or for years!
- Swelling
- Redness
- Pain
- Blurry vision
- Floaters in your vision
- Light sensitivity
Risk Factors for Uveitis
Uveitis typically affects people age 20-50. People with autoimmune or inflammatory disorders may be susceptible to developing uveitis. Smoking can increase your risk of developing uveitis.
Treatment for Uveitis
Uveitis can affect the front, middle, back or all three parts of the uvea. Our team at Atwal Eye Care will focus on reducing the inflammation in your eye through medications to reduce inflammation (prescription eye drops), antibiotics to treat infections or medications to strengthen your immune system. In more severe cases, it may be necessary to perform surgery to remove some of the vitreous gel inside your eye (vitrectomy) or insert a device into your eye that will continuously release medication to treat your condition.
Vitrectomy
Vitrectomy is a procedure that is commonly performed to treat conditions that are impacting the retina, the light-sensitive tissue that lines the inside back part of the eye. Vitrectomy surgery is done to remove the vitreous gel, a clear, jelly-like substance that fills the inside of the eye. This procedure is typically performed under local anesthesia, but you may be put to sleep with general anesthesia depending on your unique health conditions.
The vitreous gel may be removed to allow direct access to the retina to address any issues that may exist. After the retina has been appropriately treated, the space between the front and back of the eye must be filled. In many cases, it is filled with a gas bubble. Sometimes, silicone oil or a saline-type solution is inserted into the space.
Eye Conditions That May Require Vitrectomy
Certain eye conditions that damage the retina should be corrected as quickly as possible to help reduce the risk of permanent vision loss.
- Diabetic retinopathy
- Detached retina
- Macular pucker or hole
- Certain problems after cataract surgery
- Eye infection
- Severe eye injury
Your vision may not become perfect after a vitrectomy; our doctors will explain realistic expectations for your results.
Vitrectomy Recovery
Your doctor may prescribe antibiotic eye drops to help prevent infection and we will ask that you wear an eye patch for a couple of days to promote healing. You will receive instructions on how to maintain a body position that supports the gas bubble, silicone oil or saline solution that has been inserted into your eyes. Certain activities should be avoided as your eyes heal such as reading, driving, smoking, lifting objects over five pounds, bending over and any type of strenuous activity. Full recovery may take 4-6 weeks.
Risk Factors for Vitrectomy
Complications with vitrectomy are rare, but it is possible to experience side effects such as infection, inflammation, bleeding, swelling, vision changes, elevated eye pressure, increased rate of cataract growth and more. Your doctor will discuss these risks with you in detail prior to your surgery.